Heart disease doesn’t discriminate. It’s the leading cause of death for several populations, including white people, Hispanics, and Black people. Almost half of Americans are at risk for heart disease, and the numbers are rising. Learn more about the increase in heart disease rates.
While heart disease can be deadly, it’s also preventable in most people. By adopting healthy lifestyle habits early, you can potentially live longer with a healthier heart.
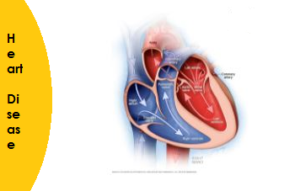
The term “heart disease” is often used interchangeably with the term “cardiovascular disease.” Cardiovascular disease generally refers to conditions that involve narrowed or blocked blood vessels that can lead to a heart attack,
Different types of heart disease?
Heart disease encompasses a wide range of cardiovascular problems. Several diseases and conditions fall under the umbrella of heart disease. Types of heart disease include:
- Arrhythmia. An arrhythmia is a heart rhythm abnormality.
- Atherosclerosis. Atherosclerosis is a hardening of the arteries.
- Cardiomyopathy. This condition causes the heart’s muscles to harden or grow weak.
- Congenital heart defects. Congenital heart defects are heart irregularities that are present at birth.
- Coronary artery disease (CAD). CAD is caused by the buildup of plaque in the heart’s arteries. It’s sometimes called ischemic heart disease.
- Heart infections. Heart infections may be caused by bacteria, viruses, or parasites.
The term cardiovascular disease may be used to refer to heart conditions that specifically affect the blood vessels.
1.What are the symptoms of heart disease?
Different types of heart disease may result in a variety of different symptoms.
Arrhythmias
Arrhythmias are abnormal heart rhythms. The symptoms you experience may depend on the type of arrhythmia you have — heartbeats that are too fast or too slow. Symptoms of an arrhythmia include:
- lightheadedness
- fluttering heart or racing heartbeat
- slow pulse
- fainting spells
- dizziness
- chest pain
Atherosclerosis
Atherosclerosis reduces blood supply to your extremities. In addition to chest pain and shortness of breath, symptoms of atherosclerosis include:
- coldness, especially in the limbs
- numbness, especially in the limbs
- unusual or unexplained pain
- weakness in your legs and arms
Congenital heart defects
Congenital heart defects are heart problems that develop when a fetus is growing. Some heart defects are never diagnosed. Others may be found when they cause symptoms, such as:
- blue-tinged skin
- swelling of the extremities
- shortness of breath or difficulty breathing
- fatigue and low energy
- irregular heart rhythm
Coronary artery disease (CAD)
CAD is plaque buildup in the arteries that move oxygen-rich blood through the heart and lungs. Symptoms of CAD include:
- chest pain or discomfort
- a feeling of pressure or squeezing in the chest
- shortness of breath
- nausea
- feelings of indigestion or gas
Cardiomyopathy
Cardiomyopathy is a disease that causes the muscles of the heart to grow larger and turn rigid, thick, or weak. Symptoms of this condition include:
- fatigue
- bloating
- swollen legs, especially ankles and feet
- shortness of breath
- pounding or rapid pulse
Heart infections
The term heart infection may be used to describe conditions such as endocarditis or myocarditis. Symptoms of a heart infection include:
- chest pain
- chest congestion or coughing
- fever
- chills
- skin rash
Read more about the signs and symptoms of heart disease.
2.What are the symptoms of heart disease in women?
Women often experience different signs and symptoms of heart disease than men, specifically with regards to CAD and other cardiovascular diseases.
In fact, a 2003 study looked at the symptoms most often seen in women who’d experienced a heart attack. The top symptoms didn’t include “classic” heart attack symptoms such as chest pain and tingling. Instead, the study reported that women were more likely to say they experienced anxiety, sleep disturbances, and unusual or unexplained fatigue.
What’s more, 80 percent of the women in the study reported experiencing these symptoms for at least one month before their heart attack occurred.
Symptoms of heart disease in women can also be confused with other conditions, such as depression, menopause, and anxiety.
Common heart disease symptoms in women include:
- dizziness
- paleness
- shortness of breath or shallow breathing
- lightheadedness
- fainting or passing out
- anxiety
- nausea
- vomiting
- jaw pain
- neck pain
- back pain
- indigestion or gaslike pain in the chest and stomach
- cold sweats
Read more about the common signs and symptoms of heart disease in women — and find out why many women say they wouldn’t call 911 if they thought they were having a heart attack.
3.What causes heart disease?
Heart disease is a collection of diseases and conditions that cause cardiovascular problems. Each type of heart disease is caused by something entirely unique to that condition. Atherosclerosis and CAD result from plaque buildup in the arteries. Other causes of heart disease are described below.
Arrhythmia causes
Causes of an abnormal heart rhythm include:
- diabetes
- CAD
- heart defects, including congenital heart defects
- medications, supplements, and herbal remedies
- high blood pressure (hypertension)
- excessive alcohol or caffeine use
- substance use disorders
- stress and anxiety
- existing heart damage or disease
Congenital heart defect causes
This heart disease occurs while a baby is still developing in the womb. Some heart defects may be serious and diagnosed and treated early. Some may also go undiagnosed for many years.
Your heart’s structure can also change as you age. This can create a heart defect that may lead to complications and problems.
Cardiomyopathy causes
Several types of cardiomyopathy exist. Each type is the result of a separate condition.
- Dilated cardiomyopathy. It’s unclear what causes this most common type of cardiomyopathy, which leads to a weakened heart. It may be the result of previous damage to the heart, such as the kind caused by drugs, infections, and heart attack. It may also be an inherited condition or the result of uncontrolled blood pressure.
- Hypertrophic cardiomyopathy. This type of heart disease leads to a thicker heart muscle. It’s usually inherited.
- Restrictive cardiomyopathy. It’s often unclear what leads to this type of cardiomyopathy, which results in rigid heart walls. Possible causes may include scar tissue buildup and a type of abnormal protein buildup known as amyloidosis.
Heart infection causes
Bacteria, parasites, and viruses are the most common causes of heart infections. Uncontrolled infections in the body can also harm the heart if they’re not properly treated.
4.What are some risk factors for heart disease?
There are many risk factors for heart disease. Some are controllable, and others aren’t. The CDC says that around 47 percentTrusted Source of Americans have at least one risk factor for heart disease. Some of these risk factors include:
- high blood pressure
- high cholesterol and low levels of high-density lipoprotein (HDL), the “good” cholesterol
- smoking
- obesity
- physical inactivity
Smoking, for example, is a controllable risk factor. People who smoke double their risk of developing heart disease, according to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
People with diabetes may also be at higher risk for heart disease because high blood glucose levels increase the risk of:
- angina
- heart attack
- stroke
- CAD
If you have diabetes, it’s essential to control your glucose to limit your risk for developing heart disease. The American Heart Association (AHA) reports that people who have both high blood pressure and diabetes double their risk for cardiovascular disease.
Risk factors you can’t control
Other risk factors for heart disease include:
- family history
- ethnicity
- sex
- age
Although these risk factors aren’t controllable, you may be able to monitor their effects. According to the Mayo Clinic, a family history of CAD is especially concerning if it involved a:
- male relative under 55 years old, such as a father or brother
- female relative under 65 years old, such as a mother or sister
Non-Hispanic blacks, non-Hispanic whites, and people of Asian or Pacific Island heritage have a higher risk than Native Alaskans or Native Americans. Also, men are at greater risk for heart disease than women. In fact, the CDC estimates between 70 and 89 percentTrusted Source of all cardiac events in the United States occur in men.
Finally, your age can increase your risk for heart disease. From ages 20 to 59, men and women are at a similar risk for CAD. After age 60, however, the percentage of men affected rises to between 19.9 and 32.2 percent. Only 9.7 to 18.8 percent of women that age are affected.
Learn more about risk factors for CAD.
How is heart disease diagnosed?
Your doctor may order several types of tests and evaluations to make a heart disease diagnosis. Some of these tests can be performed before you ever show signs of heart disease. Others may be used to look for possible causes of symptoms when they develop.
Physical exams and blood tests
The first thing your doctor will do is perform a physical exam and take an account of the symptoms you’ve been experiencing. Then they’ll want to know your family and personal medical history. Genetics can play a role in some heart diseases. If you have a close family member with heart disease, share this information with your doctor.
Blood tests are frequently ordered. This is because they can help your doctor see your cholesterol levels and look for signs of inflammation.
Noninvasive tests
A variety of noninvasive tests may be used to diagnose heart disease.
- Electrocardiogram (ECG or EKG). This test can monitor your heart’s electrical activity and help your doctor spot any irregularities.
- Echocardiogram. This ultrasound test can give your doctor a close picture of your heart’s structure.
- Stress test. This exam is performed while you complete a strenuous activity, such as walking, running, or riding a stationary bike. During the test, your doctor can monitor your heart’s activity in response to changes in physical exertion.
- Carotid ultrasound. To get a detailed ultrasound of your carotid arteries, your doctor may order this ultrasound test.
- Holter monitor. Your doctor may ask you to wear this heart rate monitor for 24 to 48 hours. It allows them to get an extended view of your heart’s activity.
- Tilt table test. If you’ve recently experienced fainting or lightheadedness when standing up or sitting down, your doctor may order this test. During it, you’re strapped to a table and slowly raised or lowered while they monitor your heart rate, blood pressure, and oxygen levels.
- CT scan. This imaging test gives your doctor a highly-detailed X-ray image of your heart.
- Heart MRI. Like a CT scan, a heart MRI can provide a very detailed image of your heart and blood vessels.
Invasive tests
If a physical exam, blood tests, and noninvasive tests aren’t conclusive, your doctor may want to look inside your body to determine what’s causing any unusual symptoms. Invasive tests may include:
- Cardiac catheterization and coronary angiography. Your doctor may insert a catheter into your heart through the groin and arteries. The catheter will help them perform tests involving the heart and blood vessels. Once this catheter is in your heart, your doctor can perform a coronary angiography. During a coronary angiography, a dye is injected into the delicate arteries and capillaries surrounding the heart. The dye helps produce a highly detailed X-ray image.
- Electrophysiology study. During this test, your doctor may attach electrodes to your heart through a catheter. When the electrodes are in place, your doctor can send electric pulses through and record how the heart responds.
Read more about the tests that are used to diagnose heart disease.
5.What treatments are available for heart disease?
Treatment for heart disease largely depends on the type of heart disease you have as well as how far it has advanced. For example, if you have a heart infection, your doctor is likely to prescribe an antibiotic.
If you have plaque buildup, they may take a two-pronged approach: prescribe a medication that can help lower your risk for additional plaque buildup and look to help you adopt healthy lifestyle changes.
Treatment for heart disease falls into three main categories:
Lifestyle changes
Healthy lifestyle choices can help you prevent heart disease. They can also help you treat the condition and prevent it from getting worse. Your diet is one of the first areas you may seek to change.
A low-sodium, low-fat diet that’s rich in fruits and vegetables may help you lower your risk for heart disease complications. One example is the Dietary Approaches to Stop Hypertension (DASH) diet.
Likewise, getting regular exercise and quitting tobacco can help treat heart disease. Also look to reduce your alcohol consumption.
Medications
A medication may be necessary to treat certain types of heart disease. Your doctor can prescribe a medication that can either cure or control your heart disease. Medications may also be prescribed to slow or stop the risk for complications. The exact drug you’re prescribed depends on the type of heart disease you have. Read more about the drugs that may be prescribed to treat heart disease.
Surgery or invasive procedures
In some cases of heart disease, surgery or a medical procedure is necessary to treat the condition and prevent worsening symptoms.
For example, if you have arteries that are blocked entirely or almost completely by plaque buildup, your doctor may insert a stent in your artery to return regular blood flow. The procedure your doctor will perform depends on the type of heart disease you have and the extent of damage to your heart.
6.How can I prevent heart disease?
Some risk factors for heart disease can’t be controlled, like your family history, for example. But it’s still important to lower your chance of developing heart disease by decreasing the risk factors that you can control.
Aim for healthy blood pressure and cholesterol numbers
Having healthy blood pressure and cholesterol ranges are some of the first steps you can take for a healthy heart. Blood pressure is measured in millimeters of mercury (mm Hg). A healthy blood pressure is considered less than 120 systolic and 80 diastolic, which is often expressed as “120 over 80” or “120/80 mm Hg.” Systolic is the measurement of pressure while the heart is contracting. Diastolic is the measurement when the heart is resting. Higher numbers indicate that the heart is working too hard to pump blood.
Your ideal cholesterol level will depend on your risk factors and heart health history. If you’re at a high risk of heart disease, have diabetes, or have already had a heart attack, your target levels will be below those of people with low or average risk.
Find ways to manage stress
As simple as it sounds, managing stress can also lower your risk for heart disease. Don’t underestimate chronic stress as a contributor to heart disease. Speak with your doctor if you’re frequently overwhelmed, anxious, or are coping with stressful life events, such as moving, changing jobs, or going through a divorce.
Embrace a healthier lifestyle
Eating healthy foods and exercising regularly are also important. Make sure to avoid foods high in saturated fat and salt. Doctors recommend 30 to 60 minutes of exerciseTrusted Source on most days for a total of 2 hours and 30 minutes each week. Check with your doctor to make sure you can safely meet these guidelines, especially if you already have a heart condition.
If you smoke, stop. The nicotine in cigarettes causes blood vessels to constrict, making it harder for oxygenated blood to circulate. This can lead to atherosclerosis.
Learn more about ways you can lower your risk for and possibly prevent heart disease.
7.What lifestyle changes does heart disease require?
If you’ve recently received a heart disease diagnosis, talk to your doctor about steps you can take to stay as healthy as possible. You can prepare for your appointment by creating a detailed list of your everyday habits. Possible topics include:
- medications you take
- your regular exercise routine
- your typical diet
- any family history of heart disease or stroke
- personal history of high blood pressure or diabetes
- any symptoms you’re experiencing, such as a racing heart, dizziness, or lack of energy
Seeing your doctor regularly is just one lifestyle habit you can take up. If you do, any potential issues can be caught as early as possible. Certain risk factors, such as high blood pressure, may be addressed with medications to lower your risk of heart disease.
Your doctor may also provide tips for:
- quitting smoking
- controlling blood pressure
- exercising regularly
- maintaining healthy cholesterol levels
- losing weight if you’re overweight
- eating healthy
Making these changes all at once might not be possible. Discuss with your healthcare provider which lifestyle changes will have the biggest impact. Even small steps toward these goals will help keep you at your healthiest.